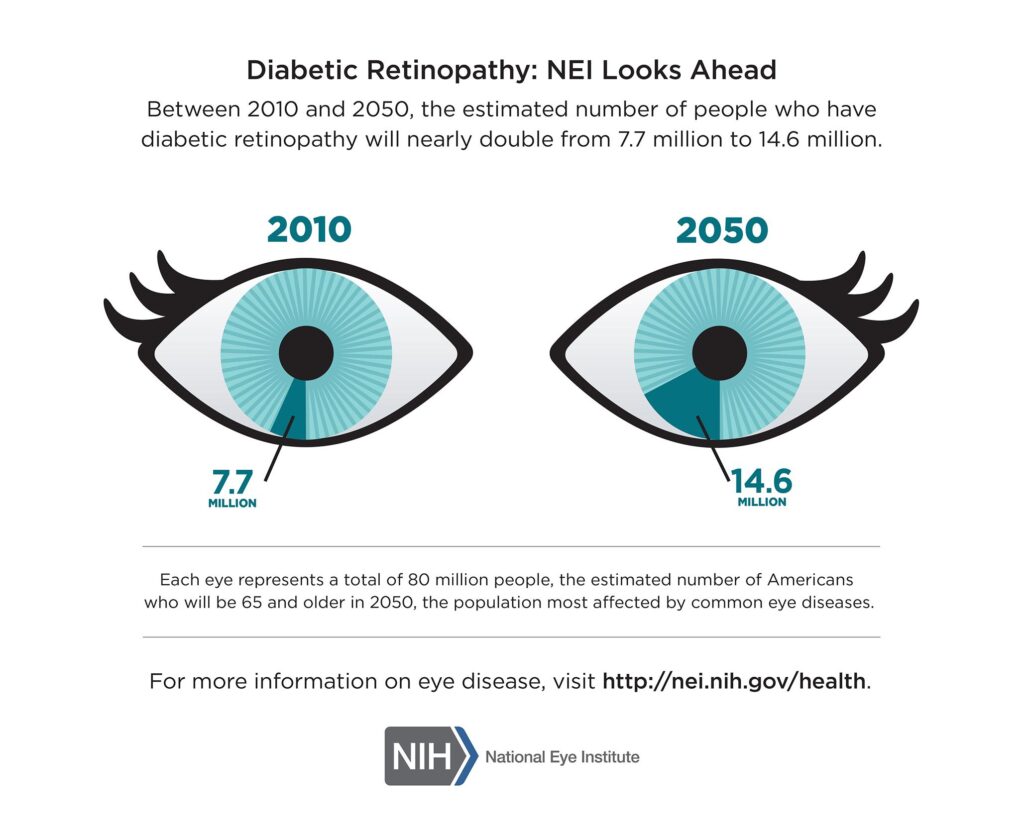
November is Diabetic Eye Disease Awareness Month, a time when we shine a spotlight on the lesser-known consequences of diabetes, a condition affecting millions worldwide. While diabetes primarily involves managing blood sugar levels, it can also silently threaten our eyesight.
Diabetes is a chronic condition that affects millions of people worldwide. While many are familiar with the impact diabetes can have on the body, not everyone is aware of the potential consequences for one of our most precious senses: our eyes. Diabetic eye disease is a term used to describe a group of eye conditions that can develop in individuals with diabetes. In this blog post, we will delve into what diabetic eye disease is, its different forms, causes, symptoms, and the importance of regular eye exams in managing this potentially sight-threatening condition.
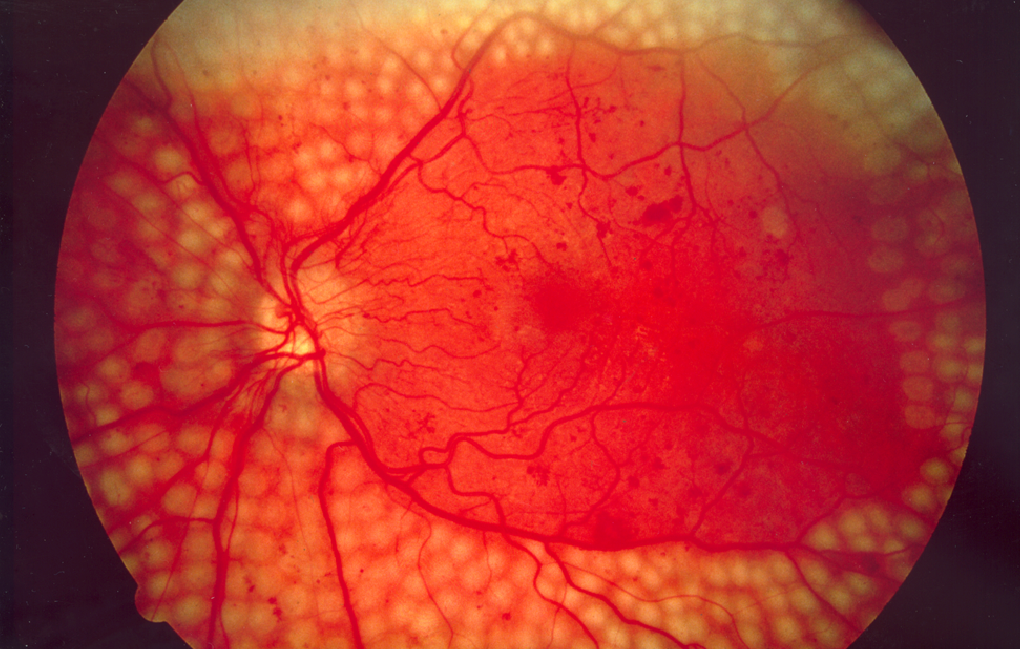
Diabetic eye disease, also known as diabetic retinopathy , encompasses a range of eye conditions that result from prolonged high blood sugar levels in individuals with diabetes. These conditions can affect various parts of the eye, with the most severe being diabetic macular edema and proliferative diabetic retinopathy.
- Diabetic Macular Edema (DME): DME occurs when fluid accumulates in the macula, the part of the eye responsible for central vision. It can lead to blurred or distorted vision and is a common cause of vision loss in people with diabetes.
- Proliferative Diabetic Retinopathy (PDR): PDR is a more advanced stage of diabetic retinopathy. It happens when abnormal blood vessels start growing in the retina, potentially causing retinal detachment and severe vision loss.
Risk Factors
The primary cause of diabetic eye disease is consistently high blood sugar levels, which can damage the small blood vessels in the retina, leading to vision problems. Several risk factors can increase the likelihood of developing this condition:
- Duration of Diabetes: The longer a person has diabetes, the higher the risk of developing diabetic eye disease.
- Poorly Controlled Blood Sugar: Fluctuations in blood sugar levels, particularly when they are not well managed, increase the risk.
- High Blood Pressure: Hypertension can exacerbate the effects of diabetes on the eyes.
- High Cholesterol: Elevated cholesterol levels may contribute to the condition’s progression.
- Pregnancy: Diabetic retinopathy can develop or worsen during pregnancy, especially in women with gestational diabetes.
Symptoms of Diabetic Eye Disease
In the early stages, diabetic eye disease may not exhibit any noticeable symptoms. As the condition progresses, individuals may experience:
- Blurred or Distorted Vision: Objects may appear blurry or distorted, particularly in the central field of vision.
- Floaters and Spots: The appearance of small specks or spots in your field of vision.
- Difficulty Seeing at Night: Reduced ability to see in low light conditions.
- Loss of Color Vision: Colors may appear less vibrant or distinct.
- Vision Loss: In advanced stages, vision loss can occur and may be irreversible.
Diabetic retinopathy is often asymptomatic until it reaches an advanced stage, which is why regular eye examinations are crucial for those with diabetes. An eye doctor can detect early signs of the condition and recommend appropriate treatments to prevent further vision loss. Managing diabetes through lifestyle changes, medication, and blood sugar control is also essential in minimizing the risk of developing diabetic retinopathy.
Diabetic eye disease is a potentially sight-threatening complication of diabetes. Understanding the causes, symptoms, and risk factors, and regularly monitoring your eye health through comprehensive eye exams can help you catch the condition in its early stages and receive prompt treatment. With proper management of diabetes and proactive care, you can reduce the risk of vision loss and preserve the health of your eyes, allowing you to enjoy a better quality of life despite living with diabetes.