Corneal Cross-linking for Adults
Therapy for patients suffering from keratoconus

FOR APPOINTMENTS CALL:
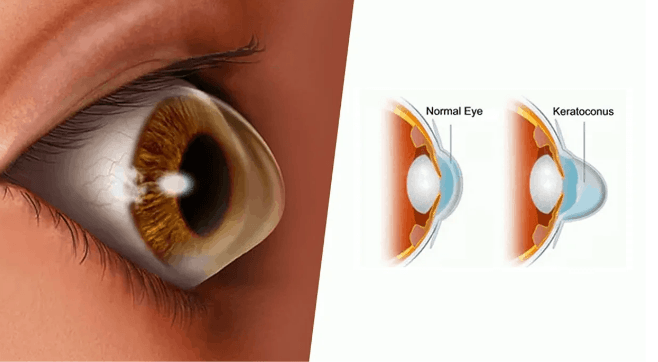
Washington University Ophthalmologists now offer outpatient corneal collagen crosslinking therapy for adults. Corneal collagen cross-linking is an innovative treatment for keratoconus and certain corneal ectatic disorders. Keratoconus is a progressive eye condition that causes the cornea to thin and bulge, leading to vision distortion and impairment. Collagen cross-linking, or CXL, offers hope to individuals affected by this condition by halting its progression and improving visual outcomes.
What is corneal cross-linking (CXL) and how does it work?
Collagen cross-linking is an innovative treatment that aims to halt the progression of keratoconus and improve visual outcomes. It is a minimally invasive procedure that involves the application of a photosensitizing agent called riboflavin to the cornea, followed by exposure to ultraviolet light. This combination helps strengthen the collagen fibers in the cornea, enhancing its structural integrity.
What is keratoconus and who is at risk?
Keratoconus is an eye condition characterized by the thinning and bulging of the cornea, which is the clear, dome-shaped surface that covers the front of the eye. This abnormal shape of the cornea can cause distorted vision, nearsightedness, and astigmatism.
While the exact cause of keratoconus is not yet fully understood, various factors are associated with an increased risk of developing the condition.
These risk factors include:
- Genetic Predisposition: Keratoconus may run in families, suggesting a genetic component to its development. If you have a close family member with keratoconus, your risk of developing it may be higher.
- Eye Rubbing: Frequent and vigorous eye rubbing is believed to contribute to the development and progression of keratoconus. Rubbing the eyes excessively can lead to thinning of the cornea and increase the risk of progression.
- Atopic Diseases: Certain allergic or atopic conditions, such as asthma, eczema, and hay fever, have been linked to an increased risk of keratoconus. The exact relationship between these diseases and keratoconus is not fully understood.
- Connective Tissue Disorders: Some connective tissue disorders, such as Ehlers-Danlos syndrome, Marfan syndrome, and Down syndrome, have been associated with a higher risk of developing keratoconus.
- Chronic Eye Irritation: Chronic eye inflammation or irritation, such as from long-term contact lens wear, can potentially contribute to the development of keratoconus.
It is important to note that having one or more of these risk factors does not guarantee that someone will develop keratoconus. Conversely, individuals without any apparent risk factors can also develop the condition. If you experience symptoms such as blurred or distorted vision, sudden changes in your prescription, or increased sensitivity to light, it is important to consult with an eye care professional for an accurate diagnosis and appropriate management.
Frequently Asked Questions
Adults 14 or older with progressive keratoconus or ectasia, without any contraindications to healing, are good candidates for crosslinking.
Corneal cross-linking can help halt or slow the progression of keratoconus, potentially reducing the need for more invasive procedures like corneal transplants.
Corneal crosslinking has been shown to be a safe and effective procedure when performed by experienced eye care professionals. As with any medical procedure, there are potential risks and side effects, which should be discussed with your eye doctor.
Recovery from corneal cross-linking typically involves a few days of discomfort, light sensitivity, and blurry vision. Most patients can resume normal activities within a week, although it may take up to a month for vision to return to baseline.
Corneal cross-linking is intended to provide long-term stabilization of the cornea. While additional treatments may be necessary in some cases, many patients experience lasting benefits from a single procedure.
Coverage for corneal cross-linking varies depending on the patient’s insurance plan and the specific circumstances. Some insurance companies may cover the procedure for patients with progressive keratoconus, while others may consider it investigational or cosmetic.
The iPath360 program by Glaukos is a service to help keratoconus patients with reimbursement questions, prescription assistance and the possibility of financial assistance for eligible patients.
Providers

Jennifer Enright, MD, PhD
Assistant Professor, Ophthalmology and Visual Sciences
- Email: enrightj@wustl.edu

Praneetha Thulasi, MD
Assistant Professor, Ophthalmology and Visual Sciences
- Email: thulasi@wustl.edu
Locations
1. Washington University Eye Center- Center for Outpatient Health
Previously located in the Center for Advanced Medicine.
- Physical Address: 4901 Forest Park Avenue, St. Louis, MO, United States
-
Mailing Address:
6th Floor
- Phone: 314-362-3937
- Fax: 866-505-8818
Full service adult eye center.