Gordon Lab
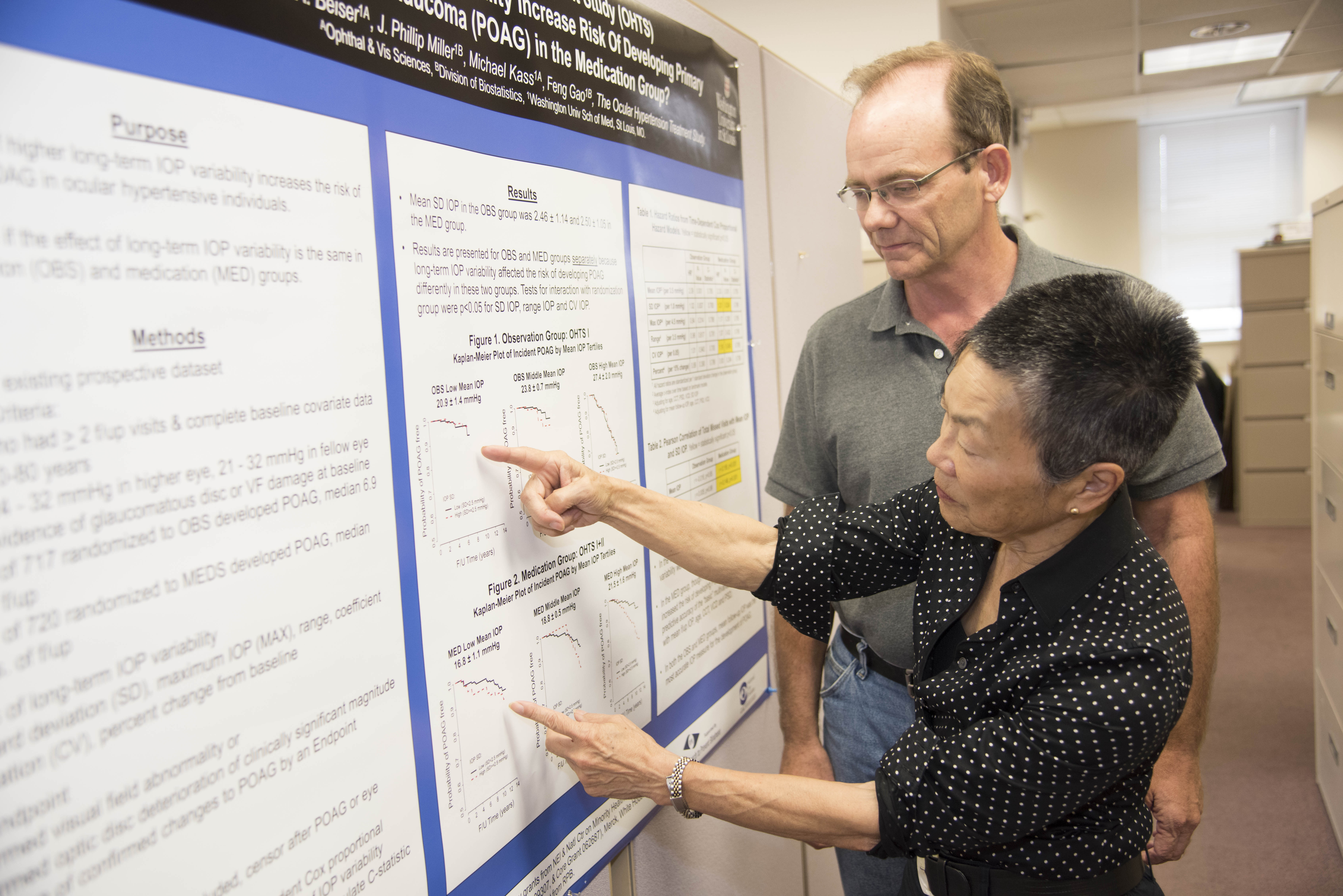
Mae Gordon, PhD, Professor, Ophthalmology and Visual Sciences; Professor, Division of Biostatistics

Research
Biostatistics Module
Drs. Mae Gordon and Steven Kymes, Biostatistics module director and co-director respectively, provide logistical, statistical and methodological expertise in the design and statistical analysis of research studies. Drs. Gordon and Kymes collaborate on two multi-center studies and have co-authored several manuscripts since Dr. Kymes joined the Department of Ophthalmology and Visual Sciences in November 2001.
Drs. Gordon and Kymes are responsible for determination of project priorities, timetable, delegation of responsibilities, and budgetary oversight. When a request for biostatistical assistance is received, Dr. Gordon or Kymes completes a brief consult by e-mail or telephone within 24-36 hours and schedules a meeting with the investigator. At the initial meeting attended by both Drs. Gordon and Kymes, a performance plan is agreed upon that specifies hypotheses to be tested, independent and dependent variables and covariates, deliverables, responsible parties and timetable.
Essential services provided by the Biostatistics module include:
- Expertise in the protocols and analysis of vision related tests and measures including:
- ETDRS visual acuity
- NEI-Visual Function Questionnaire
- Lens Opacification Classification Scale (used by D. Beebe, S. Bassnett, M. Petrash)
- perimetric data (Humphrey 30-2, 24-2 and SITA)
- optic disc analysis
- design and analysis of studies that utilize both eyes
- diagnostic trials
- logistical support e.g. IRB approvals, data management
Essential services provided by the Biostatistics Module to achieve the above specific aims are:
- to design and implement studies to provide planning data for R01 and U10 proposals
- to provide statistical and methodological expertise in study design and analysis of data
- to insure validity of statistical analyses and conclusions
- to train clinicians and basic scientists in research methodology and statistics
Ocular Hypertension Treatment Study (OHTS) Coordinating Center
Dr. Mae Gordon serves as principal investigator and director of the Coordinating Center for the OHTS study; a long-term, randomized controlled multi-center clinical trial. Over 1600 ocular hypertensive subjects at moderate risk of developing primary open-angle glaucoma (POAG) were randomly assigned to either close observation or a stepped medical regimen. Medical treatment consists of all commercially available topical ocular hypotensive medications.
In OHTS, 1,636 participants with intraocular pressures (IOP) of >24 mmHg and 21 mmHg and
Now that it has been proven that lowering IOP is effective in delaying or preventing POAG in ocular hypertensive individuals, it is important to determine when treatment should be initiated. OHTS has a unique opportunity to determine the penalty of delaying treatment since we have a randomized group of ocular hypertensive patients, one half of whom have been treated for 5-7 years (medication group); and one half of whom have been followed without treatment (observation group) for the same period. In the OHTS follow-on study, all participants will be offered medications. If we now treat all participants in both groups with ocular hypertensive medication, we should be able to determine if there is a penalty for waiting to institute treatment.
At the conclusion of this study, practitioners should be able to make reasonable estimates of an individual’s risk for developing POAG, as well as which patients would benefit from early medical treatment.
Specific Aims of the OHTS Follow-on Study:
- To determine if there is a long-term penalty or disadvantage for delaying treatment in ocular hypertensive individuals. All participants, regardless of original randomization group, are offered topical ocular hypotensive medications.
- To guide clinicians about the benefit (and risks) of early medical treatment.
- To determine which ocular hypertensive participants are at greater risk for developing POAG and would therefore be good candidates for early treatment
European Glaucoma Prevention Study-Ocular Hypertension Treatment Study Collaborative Analysis (EGPS-OHTS)
The EGPS-OHTS Collaborative Analysis study is designed as a meta-analysis study based on individual patient data from the two largest randomized trials to date that evaluate the efficacy of medical treatment in delaying or preventing the onset of primary open-angle glaucoma in ocular hypertensive individuals.
EGPS randomized 1,077 participants and OHTS randomized 1,636 participants. Both studies share similarities in study design and measurement protocols including centralized masked randomization, IOP measurement, corneal thickness measurement, ascertainment of POAG, and cause-specific attribution of abnormality. Baseline clinical characteristics of the EGPS and OHTS participants are also similar. The pooled EGPS and OHTS datasets will include data from 2,713 ocular hypertensive participants with a median follow-up of more than 5 years and over 245 POAG endpoints. The pooled sample will provide statistical power to test hypotheses that might not be possible with one dataset alone. Similarities in study design and baseline participant characteristics suggest that pooled analyses will be highly productive. This collaboration will not interfere with each study’s ability to analyze its own dataset.
Specific Aims:
- To improve the precision of risk coefficients for known risk factors for developing POAG such as age, IOP, cup/disc ratio and central corneal thickness and to assess whether other putative risk factors such as gender, high blood pressure, low blood pressure, heart disease and diabetes should be included in the risk model.
- To determine the risk of developing POAG (hazard ratio) at different levels of IOP over follow-up in both the medication and observation/placebo groups adjusting for baseline covariates – i.e., what is the difference in prognosis if a patient on medication achieves an IOP of 18 versus 21 mm Hg.
- To determine the predictive accuracy of transient visual field defects during follow-up for developing POAG.
- To determine the predictive accuracy of baseline Heidelberg Retina Tomograph indices or changes in these indices during follow-up for developing POAG.
Collaborative Longitudinal Evaluation of Keratoconus (CLEK)
Dr. Gordon serves as the principal investigator and director of the Coordinating Center for the CLEK study.
Keratoconus is a noninflammatory, axial, asymmetric ectasia of the cornea. There are no nonsurgical treatments or cures for keratoconus.
The objective of the CLEK Study is to characterize the progression of keratoconus over a broad spectrum of disease severity. The CLEK Study is strictly observational and does not provide intervention, treatment, or management. It can be likened to taking a clinical snapshot of the patient at one year intervals.
The CLEK Study has examined 1,209 keratoconus patients annually for eight years. The last study visit was completed August 2004.
Specific Aims:
- To describe the distribution and rate of change in visual acuity, corneal curvature, the proportion of patients developing corneal scarring, and the proportion of patients progressing to surgical intervention
- To identify what factors, eg, corneal curvature, corneal irregularity, corneal scarring, age, type of correction, are best corrected visual acuity and quality of functional visio
- To identify factors related to disease progression (corneal curvature)
- To identify factors related to presence and development of corneal scarring.
Economic Evaluation of Keratoconus in the Collaborative Longitudinal Evaluation of Keratoconus Study
Dr. Steven Kymes is principal investigator on an R03 grant in which the specific aim is to characterize the economic burden of keratoconus from the perspective of the patient and society. The economic analysis will use data from the CLEK study, a multi-center (16 clinics), observational study funded by the National Eye Institute that characterized the prognosis in keratoconus and its impact on quality of life. Analyses will evaluate data from the baseline examination and eight annual follow-up visits, including the close-out examination that included questions to ascertain the economic burden of keratonconus. 967 CLEK patients (81% of the original CLEK cohort completed the close-out visit. The economic evaluation consists of two parts. First, we will construct a decision model to describe the progression of keratoconus and related costs. Second, we will determine if disease progression is associated with economically significant events (automobile accidents, falls, and occupational accidents) that are known to be associated with impaired visual function. This project will be the first to document the costs of care borne by patients with keratoconus.
Keratoconus manifests relatively early in life, substantially magnifying its public health impact. Marked reductions in vision-related quality of life were documented among CLEK patients, whose scores in most domains of the NEI-VFQ (including mental health and social function) were similar to those reported by patients with advanced macular degeneration (stages three and four) in the Age-Related Eye Disease Study. A survey of CLEK patients found less than half had health insurance coverage for the purchase of services and supplies related to their condition. Our economic evaluation could provide health services researchers and patient advocates the evidence necessary to justify insurance coverage policy as well as advocate for research funding to improve treatment.
Since 1999 Dr. Gordon has collaborated with the Program in Occupational Therapy to characterize the impact of visual impairment on the ability of older adults to live safely and independently.
Publications
View all Mae Gordon’s NCBi publications on PubMed»
Selected from over 140 Peer-Reviewed Publications
- Gordon MO, Beiser JA, Brandt JD, Heuer DK, Higginbotham EJ, Johnson CA, Keltner JK, Miller JP, Parrish RK, Wilson MR, Kass MA for the Ocular Hypertension Treatment Study Group. The Ocular Hypertension Treatment Study: Baseline factors that predict the onset of primary open angle glaucoma. Arch Ophthalmol 2002; 120:714-720. PMID:12049575.
- Gordon MO, Steger-May K, Szczotka-Flynn L, Riley C, Joslin CE, Weissman BA, Fink BA, Edrington TB, Olafsson HE, The Collaborative Longitudinal Evaluation of Keratoconus (CLEK) Study Group. Baseline factors predictive of incident penetrating keratoplasty in keratoconus. Amer J Ophthal 2006;142(6):923-30. PMID:17157577.
- The Ocular Hypertension Treatment Study (OHTS) Group and the European Glaucoma Prevention Study (EGPS) Group. A validated prediction model for the development of primary open-angle glaucoma in individuals with ocular hypertension. Ophthalmology 2007; 114(1):10-9. PMCID:1995665.
- Kass MA, Gordon MO, Gao F, Heuer DK, Higginbotham EJ, Johnson CA, Keltner JK, Miller JP, Parrish RK, Wilson MR, and the Ocular Hypertension Treatment Study (OHTS) Group. Delaying Treatment of Ocular Hypertension. Archives of Ophthalmology 2010;128(3):276-287. PMCID:3966140.
- Gordon MO, Gao Feng, Beiser JA, Miller JP, Kass MA. The 10 Year Incidence of Glaucoma Among Treated and Untreated Ocular Hypertensive Patients. Arch Ophthalmol 2011;129(12):1630-1631. PMID:22159688.
- Gao F, Miller JP, Xiong C, Beiser JA, Gordon MO. A Joint-Modeling Approach to Assess the Impact of Biomarker Variability on the Risk of Developing Clinical Outcome. Statistical Methods & Applications. 2011;20(1):83-100. PMCID:3039885.
- Bhorade AM, Perlmutter M, Chang S, Pekmezci M, Wilson B, Gordon M. Differences in vision between clinic and home the effect of lighting in older adults with and without glaucoma. JAMA Ophthalmology 2013;131:1554-62. PMCID:4377300.
- DeBaun MR, Gordon M, McKinstry RC, MD, PhD, Michael J Noetzel, MD, et. al. Transfusion for Sickle Cell Anemia and Silent Cerebral Infarcts. New England Journal of Medicine, 2014; 371 (8): 699-710. PMCID:4195437.