Jennifer Enright, MD, PhD
(Third Year Resident)
What are your future plans?
I’m staying at WashU next year as the Chief of Ophthalmic Trauma, so I’ll be staffing the consult service, attending on trauma and cataract cases and managing the didactic and wetlab curricula for the next year.
Why did you choose Ophthalmology/WashU?
I was an MD/PhD student here at WashU so I knew firsthand that we have a great, supportive culture with faculty that are truly invested in trainees. We see a wide range of complex pathology, and I knew I’d get fantastic clinical and surgical training here that would set me up well for my future career. I have a background in basic science studying retinal development, and was excited to continue doing research and apply some of the techniques I learned in graduate school to the study of diabetic retinopathy working with Rithwick Rajagopal.
What advice would you give to the new residents?
It’s a busy few years, but worth it because you get to learn so much in such a short amount of time. Be kind to yourself, each other, to the staff, and to your patients. Take advantage of the wetlab, it’s a great resource to practice so you can feel more confident in the OR. And most importantly, don’t forget to bring your chief lots of snacks 😉
Favorite memory of your residency?
Over the years I’ve accumulated fond memories and inside jokes that are too numerous to count and wouldn’t make much sense on a website but will probably still make me smile 50 years from now. However, nothing beats talking with grateful post-op patients who can see better to do the things they love to do after surgery.
How did you survive during quarantine?
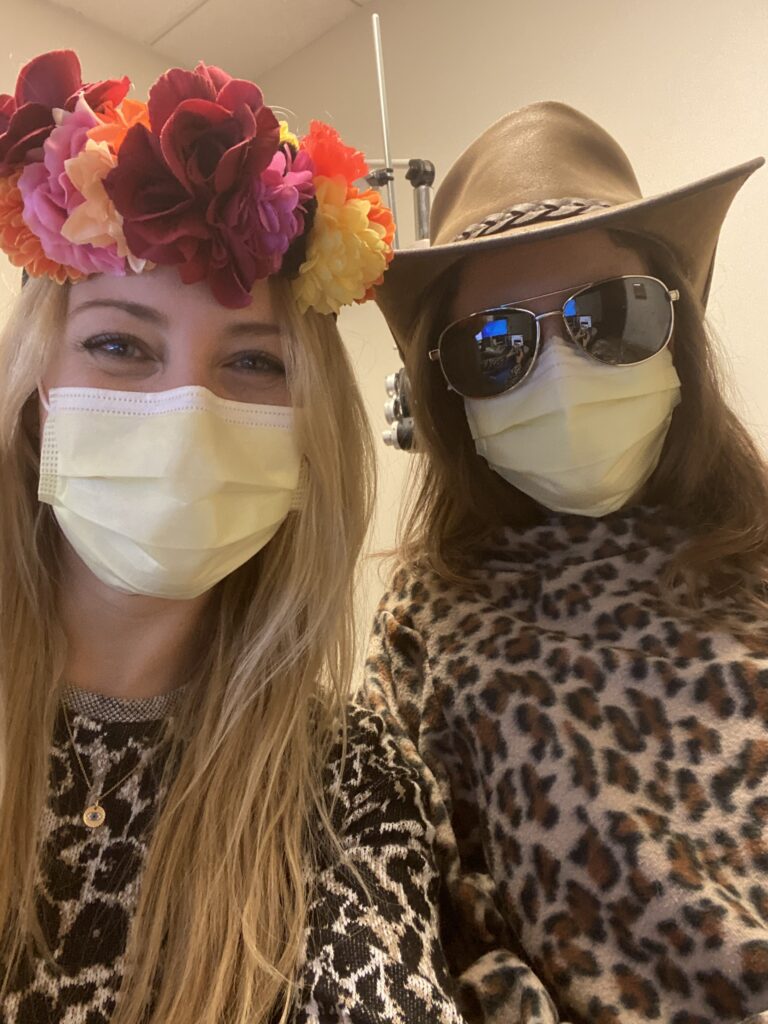
Quarantine for us was pretty short, but it was nice to have some extra time to exercise, get some writing done, and of course binge watch Tiger King on Netflix. I also spent a lot of time compulsively checking the case rate curve here and in Florida (where my parents live) and hyperventilating about the thought of managing ventilator settings, which fortunately for everyone involved I did not have to do. It was very uncertain and isolating time, but it was helpful to be able to connect with people over zoom (occasionally in costume) and really great to see everyone in clinic again as we gradually reopened.
How did you deal with the stress of your residency?
I think we’re fortunate to have a very supportive program at Wash U, and in particular I feel lucky to have had such a wonderful group of co-residents. Meeting up for a beer or a snack to commiserate about our setbacks, and to celebrate each other’s successes, has really kept me going the last three years. My significant other Tim was also a great source of support and helped provide perspective on life outside of residency when I needed it the most.
Favorite thing about living in St. Louis?
I love that St. Louis has so many different, unique neighborhoods with their own personalities, restaurant scenes and things to do. And with the cost of living being so low, it’s really easy to take advantage of it! Having Forest Park right across the street from the hospital is also great, and makes it super convenient to go for a run and get some fresh air, check out the zoo, or one of the (free!) museums.
Favorite service and why?
I really enjoyed my time on the cornea service with its busy clinic and a ton of time in the OR. Our cornea faculty Drs. Lubniewski, Huang, Margolis and Hong taught me fundamentals of surgery and patient care that will stick with me for the rest of my career, and impact how I how teach residents in the future as well.
Favorite teacher and why?
Cindy Montana– She was our chief during first year, staffed some of our very first cataract surgeries during second year, and staffs us in clinic and the OR as third year residents. I can’t imagine someone more dedicated to her work, trainees and patients and she’s been a wonderful role model to learn from throughout residency.
What did you learn in your residency that impacted you the most?
One of the hardest things we do as physicians is break bad news to patients and manage their expectations after a serious injury or diagnosis. Seeing how my attendings, fellows and seniors navigated these conversations with their patients honestly and compassionately informs how I approach these issues with my own patients now.