This Research Insight covers a series of studies supported by Mae Gordon, PhD and Michael Kass, MD that highlights the impact of a long-term clinical study, the Ocular Hypertension Treatment Study (OHTS). Together, this research—spanning more than 20 years—has revolutionized the diagnosis of primary open-angle glaucoma (POAG), its treatment, and patient outcomes.
In this series of studies, Mae Gordon, PhD and Michael Kass, MD, professors of ophthalmology at WashU Medicine, reveal key insights into patient outcomes from the pivotal, multi-site, longitudinal Ocular Hypertension Treatment Study (OHTS). Together, these clinical trials identified the crucial link between ocular hypertension and primary open-angle glaucoma (POAG). Beyond calling attention to this crucial risk factor for POAG, subsequent phases of OHTS sought to optimize ocular hypertension treatment plans, revealing a significant benefit of early intervention in high-risk patients.
Glaucoma: A Common Threat to Vision
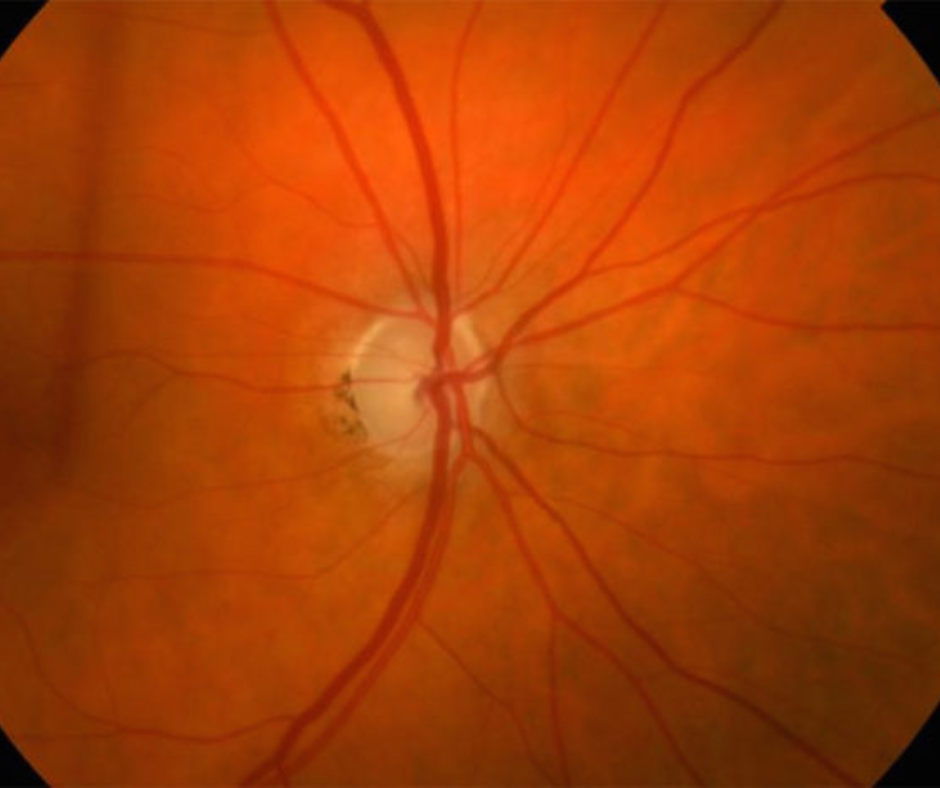
Glaucoma is a widespread disease that affects over 8 million people globally, with substantial personal and economic burdens.1 The most common subtype—POAG—is a serious health issue, as it is progressive in nature and can ultimately lead to irreversible blindness. Glaucoma threatens vision by permanently damaging the optic nerve, which is responsible for sending visual information to the brain.2 This damage is often driven by problems with fluid regulation in the eye—more specifically, a clogged drainage system.
One of the biggest challenges in treating glaucoma—particularly POAG—is that in its early stages, it is often unnoticeable to the patient.1 However, early detection is critical in slowing down its progression. Thanks in large part to the seminal work highlighted in this Vision Research Insight, we now have safe and effective treatment strategies that greatly improve long-term outcomes and preserve quality of life.
Awareness of Ocular Hypertension Is Essential to Reducing Glaucoma Risk
To understand POAG, it is important to first introduce the concept of intraocular pressure (IOP), a key indicator of eye health. Much like blood pressure, IOP is a dynamic measure of fluid regulation that can signal risk for future disease. Elevated IOP without accompanying signs of glaucoma is classified clinically as ocular hypertension, which affects an estimated 4-7% of people over 40 years nationwide.3
Awareness of IOP and ocular hypertension is paramount, given their implication in the development of POAG. Through the OHTS, researchers at WashU Medicine and its peer institutions uncovered the critical link between ocular hypertension and POAG, enabling patients and physicians to make evidence-based decisions in how they manage and treat ocular hypertension.4
Predicting the Development of POAG
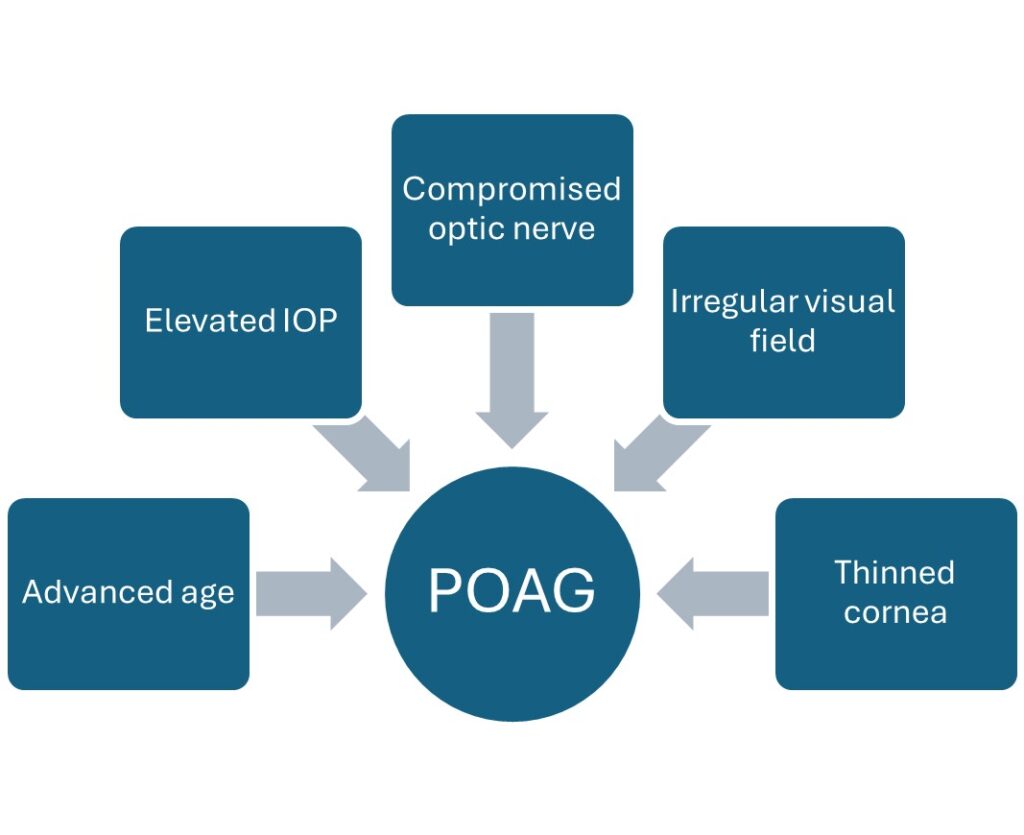
While the exact cause of POAG remains unknown, there are several largely uncontrollable factors that have been linked to its development. The OHTS introduced a 5-factor model that incorporates age, IOP, central corneal thickness, optic nerve structure, and a quantification of irregularities in the visual field to predict POAG development in an individual patient.5 Increases in all factors except corneal thickness—which was inversely related—were associated with greater POAG risk.
The OHTS evaluated how well this model predicted disease over time. Gordon and Kass found that this model reliably classifies patients into low-, medium-, and high-risk categories, with the likelihood of developing POAG over 20 years being almost 30% higher in the high-risk relative to the low-risk group.6 Accurately predicting a patient’s risk for developing POAG from baseline can allow for more informed treatment decisions over time.
Modifying Risk of POAG by Treating Ocular Hypertension
Of the 5 risk factors included in the OHTS model, only elevated IOP (i.e., ocular hypertension) can be modified by medication, making it a central focus of POAG research. Phase I of the OHTS showed that topical medication reduced IOP by at least 20% in most participants.3 Additionally, the 5-year risk of developing POAG was cut in half.
While ocular hypertension treatment proved effective, optimizing treatment plans requires balancing the overall benefit with medication costs and patients’ individual risk profiles. Phase II of OHTS explored the impact of delaying treatment, offering important insights into the role of timing in slowing progression. Although a slight penalty was observed for delaying treatment, the effect varied by baseline risk.7 Specifically, the difference between early and delayed treatment was negligible for low-risk patients but became increasingly significant with higher baseline-predicted risk. Based on these OHTS data, clinicians and patients now have access to valuable information regarding frequency of recommended examinations and tests. Low-risk, stable patients should be seen once a year, while patients in the high-risk group may need 2–3 visits per year.
Ocular Hypertension Can Be Managed Effectively to Slow POAG Progression

Contrary to disease risk factors that are at least partially lifestyle-dependent—such as high blood pressure—ocular hypertension is not reliably preventable or modifiable via behavioral changes. Rather, individuals with ocular hypertension may be genetically predisposed or have subtle variations in eye structure.5 Importantly, ocular hypertension alone does not typically manifest as noticeable symptoms; many patients have normal vision and their ocular hypertension is discovered incidentally during a routine eye exam.
Despite its silent onset, the early detection of elevated IOP is critical, cutting the risk of progressing from ocular hypertension to POAG in half.3 The OHTS has been instrumental in shaping ocular hypertension management and treatment plans worldwide, encouraging physicians to weigh a patient’s baseline risk for POAG progression, alongside other clinical and personal factors, to determine an individual patient’s optimal treatment plan.
Publications
- Weinreb RN. Glaucoma Worldwide: A Growing Concern. Glaucoma Research Foundation.
- Open-Angle Glaucoma. Glaucoma Research Foundation.
- Kass MA, Heuer DK, Higginbotham EJ, et al. The Ocular Hypertension Treatment Study: A Randomized Trial Determines That Topical Ocular Hypotensive Medication Delays or Prevents the Onset of Primary Open-Angle Glaucoma. Arch Ophthalmol. 2002. | html |
- Gordon MO, Kass MA. What We Have Learned From the Ocular Hypertension Treatment Study. Am J Ophthalmol. 2018. | html |
- Gordon MO, Beiser JA, Brandt JD, et al. The Ocular Hypertension Treatment Study: Baseline Factors That Predict the Onset of Primary Open-Angle Glaucoma. Arch Ophthalmol. 2002. | html |
- Kass MA, Heuer DK, Higginbotham EJ, et al. Assessment of Cumulative Incidence and Severity of Primary Open-Angle Glaucoma Among Participants in the Ocular Hypertension Treatment Study After 20 Years of Follow-up. JAMA Ophthalmol. 2021. | html |
- Kass MA, Gordon MO, Gao F, et al. Delaying Treatment of Ocular Hypertension. Arch Ophthalmol. 2010. | html |